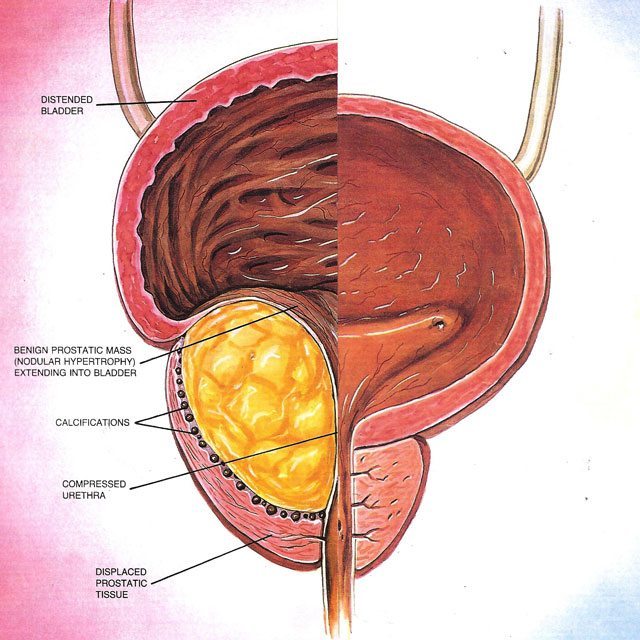
Benign Prostatic Hyperplasia (BPH)
BPH is a condition that develops in men age 40 and older. BPH is a non-cancerous enlargement of the prostate gland. The older literature also describes this as prostatism and bladder outlet obstruction (BOO).
Download BPH Symptom Evaluation Form
Symptoms associated with BPH usually present very slowly over time, rather than beginning acutely with sudden onset of symptoms. The related symptoms are: night time urination (nocturia), daytime frequency, slow urinary stream, hesitancy in initiating urination, intermittent or interrupted stream, double voiding and prolonged dribbling of urine at the end of urination.

Nocturia or nighttime urination is not the most bothersome symptom, but it does inhibit most people from getting to a good deep sleep pattern. Having to get up frequently in the middle of the night to urinate can cause daytime tiredness or chronic feelings of fatigue.
Overactive bladder symptoms include the sudden urge to urinate with or without the immediate loss of urine before you are able to make it to the bathroom. Also related is the frequency of urination; you have to make more trips to the bathroom because your body is voiding less urine from your bladder with each trip.
Dribbling, or continued flow of urine after urination is finished, is noted to increase as well. Even after men wait at the urinal or toilet, a wet spot may develop on their underwear, occasionally there is enough to show through to the outer clothing. Dribbling is a source of great embarrassment to many men, and it is something that you should discuss with your urologist.
Hesitancy is when you have a strong urge to urinate, but at the urinal, you have to wait to get your stream started. This is occasionally associated with straining to urinate or even sitting to urinate. Sitting may make living with some of these symptoms a little easier, but again, you should discuss these things with your doctor because the first line of treatment to reduce these symptoms is generally an alpha blocker medication.
Intermitency is the condition when the stream of urine cuts off before the end of urination but restarts a second or two later before urination is finished.
Double voiding is the pattern of urination where the stream stops in mid urination and restarts seconds later because a large volume of urine remained in the bladder. The second urination produces almost as much flow at the first urination. This is a sign of moderate or severe bladder outlet obstruction or BPH.
Diagnosis and Symptom Score Index of BPH
The diagnosis of BPH is usually a clinically based diagnosis made based on symptoms, that you have described in your history and explained to your doctor, a digital rectal exam (DRE) and a measurement of the post void residual urine, which is the amount of urine left in the bladder at the end of complete urination. (This is done painlessly in our office using painless ultrasound technology.) X-rays and blood tests are not typically needed. The DRE allows the Urologist to assess the size of the prostate as well as the symmetry, and consistency of the gland.
We put the BPH Symptom Score Index here for you to print out and bring to our office. Obviously, we are here to help you and our new patients print these out and bring them in on a regular basis. However, if you are not close enough to visit us the Symptom Score Index will help any urologist with their assessment of your symptoms.
Treatment of BPH
Alpha-blockers were originally used as high blood pressure medications in the 1980’s, but studies conclusively showed that they helped the prostate gland as well. Because alpha-blockers helped the prostate gland, they were refined to try and eliminate the lower blood pressure that the original alpha-blockers caused while preserving the benefits to the prostate. Alpha-blockers essentially work by relaxing the muscular fibers in the prostate itself. Examples of commonly used medications are Flomax (Tamsulosin), Uroxatral (Alfuzosin), Cardura (Doxazosin), Hytrin (Terazosin), and more recently Rapaflo. All are once daily medications. Most patients will see a difference in urination within 5-14 days. Side effects include stuffy nose, low blood pressure on rapid standing (also called orthostatic hypotension), rarely fainting, and retrograde ejaculation (“dry ejaculation” since the semen goes backwards into the bladder instead of out the penis).
The second line medications work by physically shrinking the prostate. These medications work to accomplish prostate size reduction by blocking the conversion of testosterone into dihydrotestosterone. Dihydrotestosterone is the active hormone stimulating prostatic growth. These medications leave testosterone intact thus avoiding sexual dysfunction in most people. This group of medications includes Proscar (Finasteride) and Avodart (Dutasteride). They must be taken continuously because they take months to work. (Proscar takes 6-12 months for maximal effect on the prostate size. Avodart takes only 3-6 months to work.)
There are two main pathways for the conversion of testosterone into dihydrotestosterone. About 80% of men utilize the main pathway that is blocked by the Proscar. Avodart blocks both the primary and secondary pathways. This more complete blockade accounts for its quicker onset of action.
Combinations of Flomax and Dutasteride are also available; the brand is Jalyn. The benefits of relaxation begin in a few days and help until the 3-month affect of the Dutasteride takes effect.
A Note About Supplements for Prostate Health
The original idea for the prescription medications is based on the observation that SAW Palmetto berry extract and Africanum Pygeum relieved symptoms of outlet obstruction. The European data shows these to be effective medications. However, it should be noted that the European equivalent of our FDA monitors manufacturing quality by makers of supplements while the supplement industry is nearly totally unregulated in the USA. Several independent assays of the ingredients have shown that the label does not always reflect what is in the bottle. Therefore, it is difficult to recommend any over the counter (OTC) supplement due to lack of quality control in the USA.
The way I see it, if the Mars Candy Company didn’t put 12oz of M&Ms in a 12oz bag, it should be considered fraud. If Coke didn’t put 12oz of Coke in a 12oz can, it should be considered fraud. The FDA regulates these guys, and guess what, you get what is on the label (with very little +/- but acceptable variance). Look at the recent Subway scandal. Your “foot-long” sandwich was really only 11.5 inches long. While that doesn’t sound like much, across the number of franchises, they saved a lot of money by short-changing their customers. With supplements, no one is looking. One only needs to look at the recent string of scandals in the Chinese manufacturing industry (lead found in children’s toys and jewelry, melamine chemical in plastic found in milk and milk products) to see my concerns. It has been demonstrated over and over and over via scientific testing using rigid standards of consistency that quality in OTC supplements is questionable from one manufacturer to the next, from one bottle to the next, and from one pill to the next. I suspect that if no one was looking the premium gas at the pump may actually be regular gas at an inflated price. Do you really want to take that kind of chance with your health if you have a specific medical condition that requires a very specific dose of medication to keep it under control?
Look, I have nothing personal against the use of supplements, and as a physician, I certainly need to know if you take any before deciding on a course of treatment for you. I just worry about anyone spending money (and in some cases it’s a lot of money) on these supplements. Your money may be wasted on inadequate doses, low quality ingredients, or you may simply be getting “snake oil”. (This sort of thing has been around for hundreds of years, yet it is still a modern problem because there will always be a demand for it.)
Minimally Invasive Procedures for Benign Prostatic Hyperplasia
A quick note here – any time you hear your surgeon use the term minimally invasive – listen up. Procedures and techniques have changed drastically over the past 30 years. More and more minimally invasive procedures are done now than ever before because of the quicker recovery time to the patient and the reduction of risks or complications to the patient from the procedure.
Minimally invasive surgical procedures have been employed to treat BPH in an attempt to achieve more symptomatic relief without the side effects of transurethral resection of the prostate or TURP (often referred to as a “roto-rooter” procedure). TURP is the procedure your dad and his dad were afraid of.
The two most common office based minimally invasive procedures are transurethral microwave thermotherapy (TUMT), which is the heating of the prostate with microwaves, and transurethral needle ablation (TUNA).
Both of these minimally invasive procedures use heat generated by microwaves and radio waves respectively to shrink the central portion of the prostate thus allowing the flow of urine from the bladder to the toilet once again.
Three Surgical Options for BPH are:
1. Visual Laser Ablation of the Prostate (VLAP)
VLAP is an appropriate procedure for most men with glands below 60-70cc. The size of the prostate does place some limitations on the procedure. Most normal prostate gland are small and measure about 15 cubic centimeters (cc). The range of BPH enlargement is between 30and 500cc. Luckily, most obstructing prostates are below 100cc of enlargement. It is possible on the larger 100cc glands to do these in 2 stages. This does require two different operative sessions and therefore increases the cost.
Download BPH, Symptoms and Treatments Brochure
Watch Patients discuss BPH and Treament with GreenLight laser.*
Both of these learning materials are from the AMS GreenLight website.
While most men put off prostate surgery until there are absolutely no more medical options, almost all are happy several months after the surgery and tell me how they wished they had done this sooner. Most have the stream of a much younger man and because of decreased nocturia, sleep better. This uninterrupted sleep leads to less fatigue and more energy. Most no longer have to go to every restroom they pass.
Laser ablation of the prostate, Greenlight laser or Evolve laser, is a well tolerated procedure that is usually out-patient. Most patients have a catheter for only one day. Most patients are able to drive themselves to the doctor’s office the next day. There is a recovery of 2-6 weeks depending on the degree of lifting and straining you do at work with most people being back to work in 2 weeks. This procedure does not produce any tissue samples for evaluation for cancer. If the PSA (prostatic specific antigen) is normal, no tissue is required. If the PSA is abnormal, a preoperative prostate biopsy may be obtained by your surgeon. The laser generates a very intense beam of light emitted from the end of a side-firing laser fiber. The light usually comes out the side at a 70 degree angle; this is slightly forward and protects the external urinary sphincter in the later part of the operation. The laser essentially boils the water from the tissue vaporizing the tissue. It generally seals the vessels as the resection continues thus minimizing bleeding. Usually, this results in 2-3 ounces of blood loss. Because the laser allows for the use of saline, the post TUR syndrome is avoided. Rarely is a transfusion needed, and the risk of anemia and fatigue from anemia is very small. Since there is little bleeding, the operation is usually out-patient. Most of the time, a catheter can be removed in 24 hours. I have my patients remove their catheter the following morning after surgery and to come see me in the office the next afternoon to assure proper voiding and to rule out retention of urine. One in 10 might need reinsertion of their catheter for 1-2 more days. One can care for daily living activities without fear of complications. Restrictions on lifting are for 2-6 weeks and are affected by the usage of blood thinners.
Most men worry about erectile dysfunction (ED or impotence) when considering prostate surgery for prostate enlargement or benign prostatic hyperplasia (BPH). It should be noted that this is most common with prostate cancer surgeries, and there is minimal risk with surgery for BPH. The minimally invasive procedures that generate heat such as Green Light laser or Evolve laser, TUNA (transurethral needle ablation), and transurethral microwave thermotherapy (TUMT) have a very low occurrence of ED in the 1-5% range depending on the type of surgery.
ED with surgery for BPH occurs almost exclusively in men already experiencing moderate to severe ED preoperatively. The incidence of ED is higher with a TURP possibly due to the electricity used for cutting the prostate tissue. The electricity courses out through the periprostatic nerves to a grounding pad. Open or incisional prostatectomy for BPH is also more likely to cause ED than are transurethral surgical procedures. Open surgeries are more likely to damage the nerves on the outer surface of the prostatic capsule and result in ED.
Another common concern among men undergoing prostate surgery for BPH is stress urinary incontinence or SUI. This type of incontinence occurs in only a small percentage of TURP procedures and is less common in the minimally and less invasive procedures. This is most common in men with long-standing urinary obstruction and urinary retention. This usually resolves with a few months of time. This type of problem is due to the external urinary sphincter getting lazy due to the prostatic blockage. If the prostate is blocked, then this muscle doesn’t have to work and temporarily loses some of its strength; this muscle must be exercised to stop the SUI. Kegel’s exercises help return the external urinary sphincter to its normal function and stop the stress incontinence. Kegel’s exercises are often used in women after childbirth to regain bladder control and stop postpartum SUI.
Complications of laser procedures are transient dysuria or burning with urination (6%), delayed hematuria or blood in the urine (3%), bladder neck contracture or blockage due to scar tissue (2%), and retention of urine or inability to urinate the first time the catheter is removed (1%). No incontinence or newly developed impotence was reported in most studies, and in the studies reporting ED, it is 1-3%. However, up to 26% of the sexually active men experienced retrograde ejaculation also called dry ejaculation or no ejaculation of semen postoperatively. While this does not cause any physical problem, it is psychologically stressful to some men. Retrograde ejaculation is a side effect of all prostatic surgeries and alpha-blocker medications such as Flomax/Tamsulosin.
Over the past 10 years, I have almost completely replaced transurethral resection of the prostate (TURP) in my practice with Green Light laser visual laser ablation of the prostate (VLAP). Almost everyone who is suitable for TURP is suitable for laser vaporization also called photo vaporization of the prostate (PVP).
I am just now starting to re-operate on some of the first laser patients that I did 10 years ago. The oldest patients that I have done are 89 and 93 years old. They were in urinary retention and wearing a catheter. They are both still very active.
As compared to TURP:
- The procedure is practical in most men with a prostatic gland size up to 80-100cc or about 3 ounces of tissue.
- There is significantly less blood loss with laser prostatectomies. As of 2016, none of my patients have required blood transfusion or readmission to the hospital.
- The average blood loss from a TURP is 500ml or 1 pint of blood. The transfusion rate for TURP is about 5-7% currently, but in the past, it has been much higher.
- There is no hospital stay with laser surgery of the prostate, and there almost always is a hospital stay with TURP.
- There is a rapid improvement in urine flow noted by the American Urological Association (AUA) symptom scoring after laser surgery.
- There is a shorter period of catheterization with Green Light laser PVP. The catheter is usually removed in 24 hours or less.
- There is a much quicker return to normal activity with Green Light laser versus TURP. Most men can resume most normal activity by 2 weeks. After Green Light laser, most men can drive the following day and are advised not to lift or strain for 2 weeks, or there is an increased risk of delayed bleeding. TURP patients are advised not to lift for 4-6 weeks.
- There is as little as 1% risk of developing ED in the later studies versus an initial reported rate of 3-5%.
- The laser surgery has a shorter anesthetic time, and on average, the procedure from start to finish is 60-90 minutes in the operating room.
- The Green Light laser procedure is usually shorter and therefore costs less than a TURP in most cases.
Because the fluid absorption is so much less than with a TURP, there is little or no risk of post-TUR syndrome. TUR syndrome consists of fluid overload from absorption during the TURP, congestive heart failure, and dilutional hyponatremia with confusion. Since the risk of intraoperative fluid overload is so low, older men that would be assigned to have a chronic indwelling Foley catheter with monthly catheter changes are now able to have prostate surgery.
As of 2011, there had been >200,000 Green Light laser surgeries performed worldwide.
The GOLIATH study (2014) done at 29 hospitals in 11 European countries directly compared the results of Green Light to TURP in 269 men and confirmed the safety and equivalency of laser treatment. The improvement in AUA symptom score and PSA decline in both TURP and Green Light laser were equivalent.
In conclusion, while medication is the initial main treatment for most men with BPH, once those medications no longer work, men have a safe and effective surgical procedure that is durable and as good as TURP with fewer complications and risks of ED or incontinence as compared to TURP.
2. Transurethral Resection of the Prostate (TURP)
TURP has the next longest recovery, but there is no skin incision. The TURP procedure relies on an electric cutting loop to cut out or resect the tissue. The chips, as these tissue fragments are called, are pushed into the bladder and are later retrieved for pathologic tissue evaluation. Complications include bleeding with resultant anemia and frequently require blood transfusion. The procedure usually requires several days of hospitalization and catheterization. The recovery is 6-8 weeks. The most serious intraoperative complication is the TUR syndrome. This complication results from the replacement of blood lost with a non-sodium containing fluid. This can lead to electrolyte imbalance with decreased serum sodium and potassium. This syndrome leads to swelling in the brain and confusion intra-operatively. The surgeon must stay aware of blood volume lost, the fluid used, and he must communicate well with anesthesia during the procedure. It results in a pint of blood loss in most people not requiring transfusion but does cause some temporary fatigue and weakness. The time to return to work is usually 4-6 weeks with very limited homebound activity for 1-2 weeks. Catheters are usually used 2-5 days. Required hospitalization is 1-3 days.
3. Open Prostatectomy
The best procedure for long-term symptom relief is the open removal of the central portion of the prostate. While this is the gold standard for symptom relief, it is also the most invasive, and it carries with it the longest recovery time. The open prostatectomy is now reserved for only the largest prostate glands.
This requires an incision made in the lower abdomen to access the prostate. Once the surface of the prostate is cleaned, the capsule is opened, the urethra divided, and the prostatic adenoma is enucleated. The bleeding may be quit brisk resulting in the loss of several units of blood. The capsule is closed, and a urethral Foley catheter is placed; sometimes, a suprapubic catheter is utilized as well. The normal hospitalization stay is 4-7 days with no work for 6 weeks. Bloody urine is quite common for several weeks. Blood clots causing obstruction and the inability to urinate in the first 2 weeks postoperatively are moderately common leading to ER visits for repeat catheter placements.
Prostatitis (Inflammation of the Prostate)
Prostatitis is the male equivalent of the female UTI or cystitis. Prostatitis is, however, much less common than a UTI is in women. The symptoms of both are similar and consist of new onset of frequent urination, sudden urge to urinate, an increase in nighttime urination, and possibly blood in the urine. In addition to the symptoms UTIs and prostatitis have in common, there are some that are only present with prostatitis. These consist of blood in the semen, painful ejaculation or dyspareunia (painful intercourse), new or sudden onset of erectile dysfunction (ED), or an increase in severity of mild ongoing ED. Occasionally, there will be acute urinary retention (the inability to urinate). Slowing of the stream while on medications such as Tamsulosin may occur.

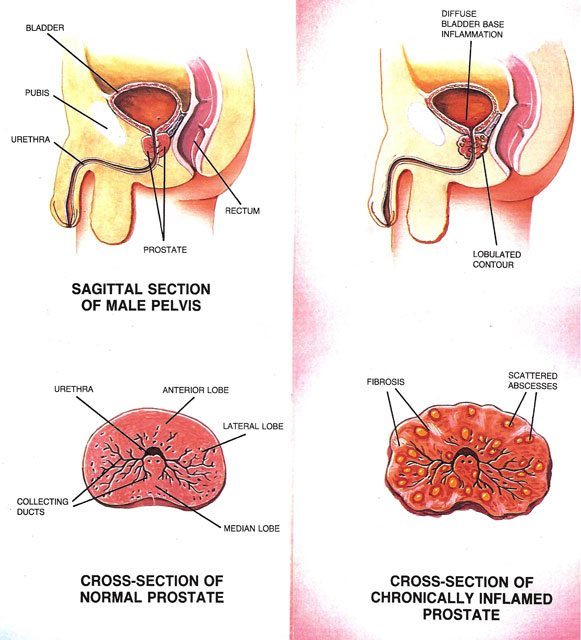
If the symptoms are ignored and the person continues to work at a strenuous job, the infection may reflux down the vas deferens and cause epididymitis. This is very painful as it results in acute swelling of the scrotum on the affected side. It becomes difficult to walk due the pain that it causes each time the testicle brushes against the thigh.
The cause of prostatitis is debatable. Many people are told it is due to a lack of frequent enough sexual activity while others are told they are too sedentary. Another group of patients that I see prostatitis in are men that work in construction. This patient group has a physically demanding job with no set starting and stopping times with an irregular break and lunch schedule.
The two stereotypical examples of people that hold their urine are truck drivers (or really anyone that has to sit for very long periods of time without getting up) and manual laborers. Many truck drivers put off urination until they have reached their destination or scheduled stop. The laborer with a full bladder keeps lifting and straining, all the while putting off urination, until either the job is done or until the next break. This requires that he hold back the urge to urinate for extended periods. Each time he stops a significant urge to go, they are pressurizing the prostatic urethra. In doing so, they set the stage for prostatic inflammation. This inflammation may turn into infection from time to time. I believe the two different people have one thing in common and that is holding their urine and delaying urination.
There are two urinary sphincter muscles that act as control mechanisms between the bladder and the outside of the body. The first one is close to the bladder and in the bladder neck. It is the internal sphincter. The internal sphincter is what keeps babies dry between diaper changes. (Without it, babies would constantly drip urine as it was produced and put in the bladder.) The external sphincter is the toilet training muscle, and it is positioned below the prostate. When you stifle urination and force the urge to urinate to go away, you are pressurizing the prostatic urethra. Sometimes, by doing this, the very acidic urine can cause inflammation of the prostate, and this can set the stage for a possible prostatitis.
Treatment consists of antibiotics, scrotal support, ice (initially), and heat (later). The time course is much different in men’s prostatitis than in women’s UTIs. Women may be treated with 3-5 or even 7 days of antibiotics depending on age, associated illness, and frequency of their UTIs. Men are treated for 2-4 weeks or even as long as 6-12 weeks. The difference is that women are treating a urine infection that empties with each trip to the toilet. The germs are diluted as they are killed by the antibiotics. The antibiotics in women are excreted in the urine as a waste product and may reach 200 times the achievable concentrations of antibiotics in the blood stream. Men, however, are treating a tissue infection and must rely on blood levels of antibiotics alone. At these lower levels of antibiotic concentrations, mean inhibitory concentrations or MIC for short, takes much longer to clear the bacteria from the tissue than it does from urine. The larger the prostate the longer it takes to clear the infection. Associated conditions such as increased post-void residual urine or incomplete empting prolong the treatment as well.
Antibiotics are merely chemicals that kill bacteria but do not harm the person taking them. Most bacteria have a favorite acid or basic environment to work in, or favorite pH. Most infected tissues are acidic or have a low pH; prostatic tissue may have a more basic pH when infected. At a pH of 7-8, the same antibiotic does not work as well as it might at an acid pH of 5-6. This also prolongs the treatment of prostatitis. The lipid membranes in the prostate may also prevent the large molecules of common antibiotics like Sulfa drugs, Bactrim, and Septra from crossing readily into the cells.
The oldest treatment (before around 1960) prior to the invention of antibiotics for prostatitis was the digital rectal prostate massage (DRE). Men would go to the doctor sometimes 2-3 times a week for a rectal massage of the prostate. The fluid expressed from the prostate would give temporary relief from the symptoms of prostatitis. This may be where the notion that regular ejaculation prevented prostatitis comes from. It surely plays into the psyche of men “needing” regular intercourse to prevent problems and infections of the prostate. A study in 2006 concluded that prostate massage did not improve outcomes for treatment of prostatitis and that antibiotics alone should be used to treat prostatitis.
The most common antibiotics used today for the treatment of prostatitis are the Quinolone antibiotics such as Cipro (Ciprofloxacin), Levaquin (Levofloxacin), Sulfamethoxazole / Trimethoprim (Bactrim, Septra), Vibramycin (Doxycycline), and occasionally Cephalosporins such as Keflex (Cephalexin)
The urologist will evaluate you for conditions predisposing you to infections. Risk factors include incomplete emptying due to urethral strictures, scarring in the tube through the penis, prostate enlargement or BPH, bladder stones, diabetes mellitus, and medications such as immunosuppressants, the most common of which are steroids and other chemotherapeutic agents. The occasional prostatitis that clears rapidly needs only an office evaluation. The recurring types need more in-depth evaluation and may require cystoscopic evaluation of the urethra, prostate, and bladder. Radiographs such as CT scanning may sometimes be a part of the evaluation.
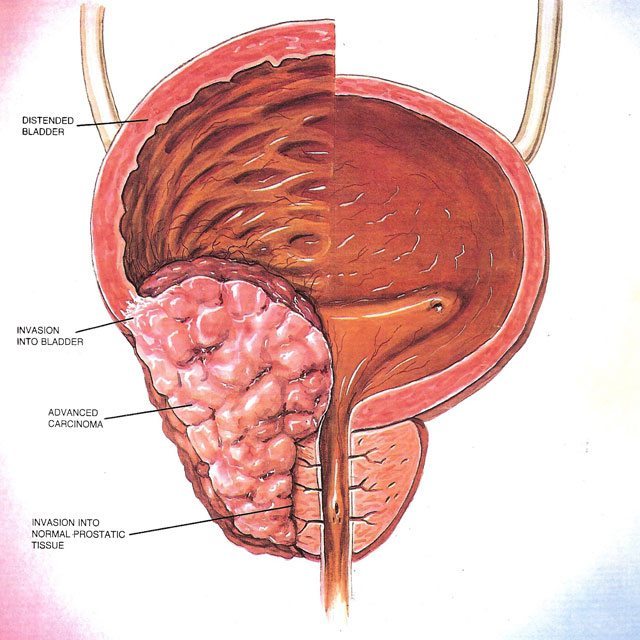
Prostate Cancer
According to the Centers for Disease Control and Prevention (CDC), the top diagnosed cancer among men in the United States is prostate cancer. In 2007, there were 223,307 men diagnosed with prostate cancer, and 29,093 men died from the disease. Prostate cancer is also the second leading cause of cancer deaths in men after lung cancer. (The top three cancers in men are lung, colon, and prostate.) Early diagnosis of cancer is the basis of all other advances in the treatment of breast cancer, cervical cancer, colon cancer, and lung cancer, and studies have shown that the earlier the these cancers are diagnosed in a patient the better the survival rate is for that patient. The CDC study I referenced earlier also added, “Since there is not enough medical evidence to decide if the potential benefits of prostate cancer screening outweigh the potential risks, the CDC supports informed decision making.”
Having seen men’s reluctance to have a digital rectal exam and the dismal history of DREs at early detection of prostate cancer, the prostatic specific antigen or PSA was invented. This has been used in conjunction with DREs over the last 20 years to find prostate cancer in its earlier form.

There are several prostatic conditions that may elevate PSA. These include benign prostatic hyperplasia or BPH, prostatitis, and prostate cancer. Larger prostates have more PSA than smaller ones. The amount of PSA per cubic centimeter or cc of prostatic tissue is called the PSA density. The PSA velocity is the amount of rise over a period of time; all of the conditions above are used to evaluate men for signs of prostate cancer. There are no early warning signs of prostate cancer. A prostate biopsy is used to obtain tissue from the gland to look for prostate cancer cells. Prostate cancer can not reliably be found on rectal exam, CT scans, or MRI.
Recently, the US Preventive Services Task Force has recommended that doctors stop using PSA as a screening tool for prostate cancer. They found no benefit in survival of men found in the early stages of prostate cancer by PSA. They alleged that screening does more harm than good. This seems contrary to what occurs in the treatment of all other cancers found in the early stages. Many primary care physicians stopped doing digital rectal exams in favor of PSA. Now that there is a recommendation to stop doing PSAs, they have not resumed DREs, thus abandoning all efforts to find prostate cancer. If your doctor is not at least discussing PSA and doing a DRE, you to ask your physician for an exam.
Breast cancer is the analogous cancer in women to prostate cancer in men. Both are mediated by hormones, estrogen in women and testosterone in men. Women receive a breast exam and a mammogram, while men need a DRE and a PSA. Family history of either of these cancers increases the risk for other family members. Some studies have suggested that the same chromosomal mutations may be responsible for both cancers. The earliest medical treatment attempts in both were manipulations of these hormones. If either a woman with a breast mass or an abnormal mammogram or a man with an abnormal DRE or PSA is found, both require biopsy for diagnosis. CT scans and MRIs are used for staging after biopsy but are not reliable enough for diagnosis. Of course, not all biopsies will be positive for cancer. In men, about 25% of people with a PSA between 4-10ng/ml will have a positive biopsy. There is a similar positive rate in breast biopsy. Now critics of PSA say that if only one is positive that the other 3 were “unnecessary”. How can they be unnecessary if there is no other test to find the cancer? In women all biopsies appear to be necessary even though many find benign breast conditions. Many women have had 2, 3, or even 4 breast biopsies in their lifetime.
Conventional wisdom says that all men have a small amount of prostate cancer, so what’s the big deal since you always “die with prostate cancer and not of prostate cancer”? In the 1960’s, the life expectancy of a male was about 65 years. So if a man with medical problems was diagnosed with cancer at age 55-60 years, it is true that he may very well die of other causes. Now that the life expectancy is 76.5 years with an upward range of 90 years, it is not true of relatively health people diagnosed at an early age (less than 70 years old). In people with a 10-15-year survival, there is a 44% reduction in deaths in the screened early stage prostate cancer group.
There are about 30,000 prostate cancer deaths each year in the USA, and there are 240,000 newly diagnosed cases of prostate cancer per year. Men over 50 years of age, the age group most at risk, make up about 25% of the male population, about 10 million men, in the USA. One man in 36 will die of his cancer. While the USPSTF found no benefit to prostate cancer screening in the USA, the ERSPS or European Randomized Study for the Screening of Prostate Cancer found a 21% decrease in the risk of death from prostate cancer in the PSA screened group. The Göteborg trial found a 40% reduction in prostate cancer death in the age group of 50-64 year olds with a 14-year survival. There has been noted to be a 44% reduction in prostate cancer related deaths in the USA over the last 20 years. The SEER data shows a 75% reduction in the presentation of men with advanced stage disease. The survival in localized prostate cancer is about 72% while the survival for metastatic disease at 10 years is only 3%. Screening has lowered the number of men presenting with advanced stage or metastatic disease by 75% over the last 20 years. Metastasis is the advanced state of a cancer where it has spread distantly from the primary site. In prostate cancer, this spread is typically to bone.
Some groups are at greater risk of prostate cancer. These include African Americans and anyone with a family history of prostate cancer. Even if random screening is found to be of no benefit to men in general, which I find unlikely given the increase in average life expectancy, targeted screening of these groups should continue.
All cancers are not aggressive. Your doctor tries to take this into account if your biopsy is positive. An informed decision to treat or watch a cancer is a complex decision best discussed with your urologist. I personally do not recommend treatment for small prostate cancers in all patients. Some patients benefit from a “wait and see” approach or watchful waiting. Watchful waiting is also called medical monitoring in some articles. This involves serial monitoring of PSA and DRE to try to pick out the cancers with the aggressive growth patterns for treatment and the slow growing ones for close monitoring. If an initially slow growing cancer changes to a more aggressive growth pattern, some people then decide to change to a treatment and quit the monitoring group.
Your urologist should help you understand that he takes into account the grade of the tumor or Gleason score, the TMN stage of the tumor, the PSA, the volume of tumor, stated as the number of cores positive for cancer from your biopsy, and whether it is unilateral or bilateral. He should consider your family history of longevity, and he should speak to your family doctor about your overall health and consider whether you will live another 10 years or more. People with multiple medical illnesses not expected to live another 10 years should seriously consider monitoring over treatment of a small, non-aggressive, prostate cancer.
The goal of treating prostate cancer is not just to cure it but to decrease the morbidity and to evaluate the decrease in the overall quality of life associated with incurable prostate cancer. The spread to bone is often quite painful. The chemical castration treatments cause significant decreases in quality of life evaluations. These treatments can routinely cause hot flashes, night sweats, muscle weakness, osteoporosis, and cognitive decline. While urologists realize that there is certainly a downside to treating prostate cancers with surgery and radiation, doing nothing is not often a good option either.
The recent discussion seems to favor going back to the pre 1980’s non PSA era when 16.9% (T1) was the percentage of early stage prostate cancer; 48% were T2. T1 is now about 50% (early stage cancer now) and 27% T2. Certainly there has to be some happy median between the treatment for all and no treatment for anyone.
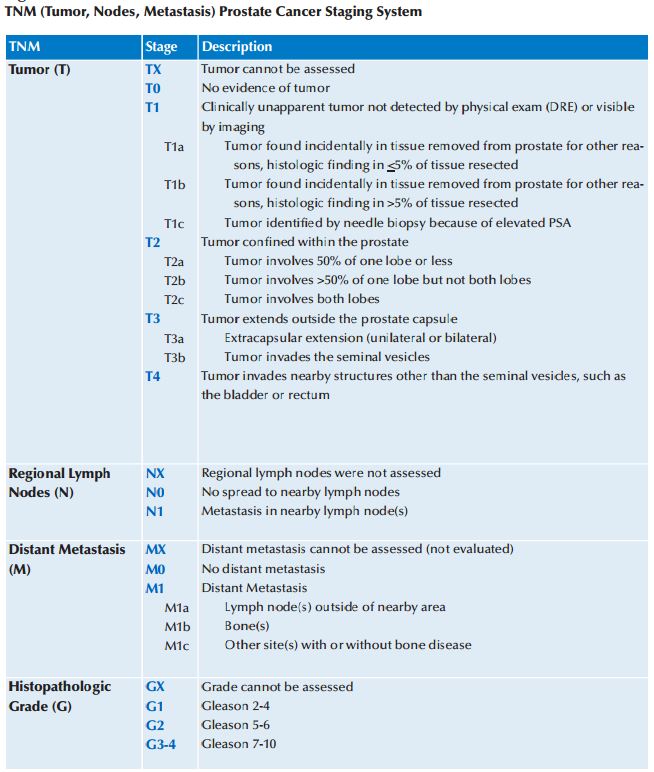
Prostate Cancer Grading
Prostate cancer is graded using the Gleason score. This score factors in a two-part grade, a nuclear grade, and a glandular grade. The glandular grade has to do with the architecture of how the glands are put together on the biopsy specimen while the nuclear grade looks at the nucleus of the individual cells for clues of how aggressive that cancer may be. An example would be a 3+4/10 or grade 7/10. The system allows for more categories to tell how aggressive the tumors usually act. A grade 3+4 is a less aggressive tumor than 4+3, although both are grade 7. The later 4+3 acts more like a grade 8/10 cancer.
Staging of Prostate Cancer
Localized Prostate Cancer
This implies that the prostate cancer is confined to the prostate gland and has not spread outside the prostatic capsule, no spread to the regional lymph nodes, or distant metastasis to bone.
Local Spread of Prostate Cancer
This is spread detected in the surgical pathology specimen and has typically spread just beyond the prostatic capsule but not into the regional lymph nodes.
Distant Spread of Prostate Cancer
This indicates spread to the lymph nodes out of the pelvis and/or into the bone.
Staging the cancer after needle biopsy utilizes a bone scan when the PSA is grater than 20.0 and the Gleason score is 8 or greater. The bone scan is a radio nucleotide scan that marks areas of bone that are abnormal and need further evaluation by standard x-rays or MRI. This typically exposes the person to less ionizing radiation than they would get using multiple plain x-rays.
Computed Tomography Scanning (CT scan, which is sometimes called a CAT scan) is used to evaluate the pelvic area for signs of pathologically enlarged lymph nodes. These are typically lymph nodes greater than 10 millimeters in diameter.
Magnetized Resonance Imaging (MRI) is currently used in staging prostate cancer, evaluating suspicious boney lesions, or for guiding prostate biopsies but not currently for diagnosing prostate cancer.
Prostate Cancer Treatment
Watchful Waiting of prostate cancer:
This act of diagnosing prostate cancer but not treating the cancer is called watchful waiting. Through mutual agreement between the patient and the urologist the patient undergoes regular DRE and PSA testing. This is most often reserved for older, sicker patients with small amounts of cancer on biopsy. They typically have lower Gleason score cancers. If the cancer shows signs of progression, then treatment may be initiated at the time of progression.
Medical Monitoring of prostate cancer:
Medical monitoring is very similar to watchful waiting, but in addition to monitoring PSA and DRE, it usually adds a follow-up prostate biopsy. If the second biopsy shows an increase in tumor volume or increase in Gleason score treatment is again discussed
External beam therapy:
External beam therapy is the use of radiation generated by a linear accelerator to produce the wavelength of radiation needed to treat the prostate cancer. This is usually given in daily fractions Monday thru Fridays for 8-8.5 weeks. It may be aided by the insertion of gold fiduciary marker seeds to guide the radiation therapy. The prostate rises when the rectum is full of stool or gas, and the bladder may change position based on its degree of fullness. The marker seeds allow the therapist to change the depth of treatment from day to day to accommodate these changes in position. This is used to avoid damage to the bladder and rectum.
Seeds/Brachytherapy:
This is the treatment of prostate cancer by insertion of radio active seeds or pellets directly into the prostate. Both Iodine 125 and Palladium 103 are used. This delivers a higher dose of radiation to the prostate than can be delivered by external beam (EBRT) with no increase in side effects.
Radiation plus Hormonal Deprivation:
Tumors with higher grades and PSAs have a greater tendency to recur. In an attempt to stop the recurrence, LH-RH (Luteinizing Hormone-Releasing Hormone) inhibitors were given to the patient before the radiation therapy. LH-RH inhibiting factors affect the pituitary to stop the release of LH. LH is the hormone that stimulates the testicle to produce the testosterone. By blocking this hormone, testosterone levels fall to 30ng/ml, which is the same as castrate testosterone levels. Starting with the LH-RH medications before onset of ERBT weakens the cancer cells and makes them more sensitive to radiation induced cell death. Initially, 3 years of LH-RH were used. Then 2 years of LH-RH plus antiandrogens were shown to be as good. Now some patients require only 3-4 months of LH-RH and antiandrogens reserving the longer course for patients with grade 8 or with a PSA greater than 20.0.
Combined EBRT and Brachytherapy:
For higher grade tumors with higher Gleason scores, higher PSAs, and more volume of tumor, the EBRT may be used to treat the area outside the prostatic capsule while using brachytherapy seeding to increase the dose to the center of the prostate gland.
Radical Prostatectomy:
This is the removal of the prostate by surgical means. The prostate is disconnected from the bladder, the prostatic urethra, and the rectum. A nerve sparing technique is to preserve the nerves responsible for erection. This avoids causing ED
Retropubic Prostatectomy:
This approaches the prostate through a small 4-5 inch incision beginning over the pubic bone at the base of the penis and extends upward. This is the approach preferred by about 90% of surgeons. Nodes can be sampled in this technique.
Perineal Prostatectomy:
This approaches the prostate through a transverse incision behind the scrotum but in front of the anus. The nerve sparing technique is also employed. Nodes cannot be sampled using this approach.
Robotic Retropubic Laparoscopic Prostatectomy:
Robotic retropubic prostatectomy utilizes a surgical robot to assist the surgeon. The advantages are that the laparoscopic approach uses a smaller incision and there is significantly less blood loss. The anastomosis or closure of the urethra to the bladder can be seen more easily. There are conflicting reports as to whether this procedure actually causes less incontinence and erectile dysfunction than does the open procedure. The learning curve for the robotic surgeon is stated to be about 100-200 cases before the rate of leaving a positive margin decreases to that of an open surgery. Many university trained surgeons now come out of training with this number of cases. The implication of a positive margin is that cancer has been left behind, and the patient may need additional therapy such as follow-up postoperative EBRT.
Incontinence
Stress versus Urge Incontinence:
Incontinence is defined as leakage of urine. There is stress incontinence such that when one coughs, sneezes, or moves suddenly urine comes out unexpectedly. This is most common after surgery and usually goes away as healing continues over 4-12 months. Treatment options include Kegel exercises to strengthen the external sphincter, biofeedback, and surgical sling procedures.
Alternately, there is urge incontinence with loss of urine accompanied by the sudden urge to urinate and the inability to stop the initiation of urine flow. Multiple medications are available for treating this problem. The most common side effects of these anticholinergic medications are dry mouth and constipation. This type of incontinence is most common after radiation therapy and most often goes away over 4-12 months.
Erectile Dysfunction (ED)
Delayed versus Immediate:
Immediate ED is found in up to 80% of prostatectomy patients. The ED improves over the first postoperative year with about 50-80% recovery in the ability to resume intercourse. The resumption of intercourse may require the use of medications such as Viagra(sildinafil), Levitra(vardenafil), or Cialis(tadalafil) Attempts to speed the return of normal erections include starting these medications in the immediate postoperative period. They usually begin as soon as 2 weeks postoperatively. Intracorporeal injection of vasoactive medications has been tried as well. Medications such as prostaglandin E1 (brand name Caverject) and Edex are used. Older mixtures of Phentolamine and Papaverine, or occasionally Trimix (a mixture of prostaglandin E1, Phentolamine and Papaverine) are the most commonly used medications. Some studies have recommended the use of vacuum erection devices for the return of erectile function.
Positive Margins on a Pathology Specimen
If the pathology specimen has a positive margin, meaning some of the cancer may have been left behind, then close follow-up with serial PSA tests are used. The first PSA is taken 6-8 weeks after the surgery. If the PSA fails to fall below the level of < 0.015ng/ml, then cancer cells are present and are producing PSA. At this point, additional treatment may be offered in the form of External Beam Radiation Therapy (EBRT). For the best results, the EBRT should be administered before the PSA reaches a level of 1.0ng/ml. Surgical removal of the prostate devitalizes a small rim of tissue around the prostate. This area dies back for several millimeters. If the margin containing the cancer was small, this zone of tissue death may kill the rest of the cancer. About 30% of positive margin patients normalize their PSA to less than 0.015ng/ml. They usually do not require EBRT treatment.
Biochemical Recurrence/ Metastasis:
A rising PSA, after it initially returned to nearly zero, is indicative of the cancer coming back. In the presence of a positive margin, a negative bone scan, and negative CT scan, it is assumed that it is a recurrence in the pelvis and probably will respond to EBRT. This rise in PSA can occur as long as 11 years after having a negative margin pathology specimen and undetectable PSA. While most recurrences are found in the first 5 years, long-term monitoring is required.
Hormonal Therapy:
Prostate cancer, much like breast cancer, is most often sensitive to hormonal deprivation therapy. The male hormone is called testosterone. Lowering of testosterone was first found to treat metastasis to bone with bone pain in the 1950s. Hormonal deprivation, in the 1950s, was accomplished by removal of the testicles otherwise known as castration. In the 1980s, Luteinizing hormone-releasing hormone inhibitors, LHRH for short, were used to block the pituitary hormone LH. The testes no longer had to be removed to treat the cancer. The medication simply turned off the production of testosterone. Several drugs are available including Lupron, Trelstar, Eligard, and Zoladex. While at first requiring monthly injections, the drugs now come as 3, 4, and 6 month preparations.
Side effects include menopause-like symptoms of hot flashes, night sweats, agitation or depression, and osteoporosis may occur.
Antiandrogens:
Some testosterone is made by the adrenal glands, and this accounts for a small portion of the total testosterone. If normal testosterone is 350 to 1,198, the castration levels are about 30ng/dl. This small amount of testosterone from the adrenal glands, may be enough to keep the cancer growing. Antiandrogens attach to the testosterone receptors and block the body’s use of the remaining available low testosterone.
Chemotherapy for Hormonal Resistance
Currently, several chemotherapies are available for patients failing standard hormonal therapy. These patients are said to have castration resistant prostate cancer and it is hormonally insensitive. Discussion of these types is beyond the scope of this article.
Taxotere (Docetaxe) l and Zytiga (Abiraterone) are the two chemotherapies given by oncologists but these are both beyond the scope of this article.