Urinary Tract Infections (commonly referred to as UTIs) are very common infections. We see more women than men for UTIs because about 40 % of women and only 12% of men will develop UTIs. (Men instead develop prostatitis, which is covered in another section.)
Urine infections in women have several names. They are essentially all describing the same thing, an infection of the bladder. The most correct term is cystitis, an infection of the bladder. These are confined to the bladder and do not ascend up the ureter to the kidneys. They are also called urine infection, bladder infection, kidney infection, and urinary tract infection (UTI).
UTI is a broad term that does not specifically single out the site of the infection. Urethritis is an infection of the urethra. The urethra is the tube from the bladder to the outside of the body.
Cystitis is the true term for an infection of the bladder.

Prostatitis is an infection of the male prostate gland. Women do not have a prostate.
Ureteritis is an infection of the ureter. This is the tube that connects the kidney to the bladder.
Pyelonephritis is a true infection of the kidney. The initial bladder infection has gained access to the ureter and traveled up all the way into the kidneys.
Urosepsis or “blood poisoning” is an infection that has invaded into the blood stream.
Symptoms of UTI
- Frequency of urination suddenly increases.
- Urgency is the sudden urge to get to the toilet for fear of incontinence.
- Dysuria is that burning sensation that occurs with urination.
- Nocturia is the need to get up in the night to urinate.
- Hematuria is the finding of blood in the urine.
- Pelvic pain occurs in women.
- Rectal pain may be found in men.
- Cloudy urine may be a sign of infection.
- Persistent urge to urinate and a feeling of fullness after urination may be present.
- Strong odor to the urine may develop.
- Feelings of incomplete emptying are common.
- Incontinence of urine is found in some people.
- Painful sex occurs in women.
- Painful ejaculation occurs in men.
- Low-grade fever < 100°F for cystitis. High fever >101°F, with chills, nausea, and vomiting in pyelonephritis.
- Elderly people may have loss of appetite and occasional mental changes or confusion.
Causes of UTI(s)
Women have several times in their life where the risk of a UTI is known to increase.
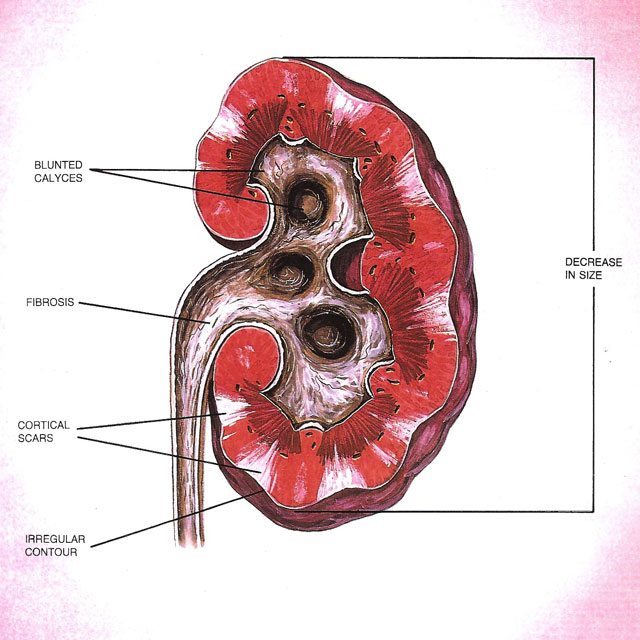
The first time for females to acquire a UTI is as a child. Children with UTIs usually need an evaluation for birth defects of the urinary system. The most common defect is ureterovesical reflux. In this situation, the insertion point of the ureter into the bladder is abnormal, and urine flows backwards into the kidney during urination. This backward or retrograde flow is called reflux.

The second time in a young woman’s life that the number of UTIs increases is with the onset of her menstrual cycle. Whether this is due to tampons and pads or hormonal changes, it is not clear.
Onset of intercourse has long been noted to cause a UTI in women. That is where the term ‘honeymoon cystitis’ comes from. Due to the position of the female urethra in the upper edge of the vagina, sex irritates the urethra and allows bacteria to enter the urethra. Since the urethra is shorter in women than men, it is easier for the bacteria to ascend into the bladder. In most women, cystitis occurs a few times and goes away. In a few cases, intercourse remains a frequent source of UTIs throughout her lifetime.
Pregnancy is noted to have an increased incidence of UTIs in some women. Whether this is hormonal, immunosuppression in the mother, or stasis in the system, it is not clear. The gravid or pregnant uterus begins to compress both ureters at about 20 weeks. This compression first affects the right kidney, and then a few weeks later it affects the left side. The pressure of the enlarged uterus upon the ureters at the pelvic brim creates hydronephrosis or back up on both kidneys.
Menopause is also noted to bring on an increase in frequency of UTIs. The degree of difficulty of treatment increases as well. The loss of estrogen has a direct effect on the health of the lining of the bladder as well as the lining of the vagina.
Evaluation
Evaluation for repeated UTIs is advised in women having more than 4 per year, one that will not clear, or with pyelonephritis.
Evaluation will include:
- Urinalysis is done to see if the symptoms are truly a UTI. Some of the other illnesses that may mimic UTIs are interstitial cystitis (IC), estrogen deficiency, and endometriosis.
- Urine cultures may be sent to the laboratory. The urine is set up to see if a bacteria grows and how many. If bacteria grow, then they are treated with different antibiotics to see which one is the most effective treatment.
- The post-void residual urine will be checked to make sure the bladder is empty. Poor emptying leads to repeated UTIs that are difficult to clear. The difficulty in clearing the UTI is due to the stagnant urine left in the bladder after each urination.
- Ultrasound or bladder scan measurement of this residual urine is non-invasive and does not require a catheter be inserted into the urethra.
- Pelvic exam looks for cystocele formation, descent of the bladder into the vagina after childbirth.
- X-ray evaluation such as renal ultrasound, intravenous pyelogram (IVP), or CT urogram may be ordered to evaluate for obstruction of the ureters, signs if old scarring from childhood reflux, stones and/or tumors.
- Cystoscopy is used to evaluate the lining of the bladder. Flexible cystoscopes are used in the office and are more comfortable than rigid cystoscopic evaluations.
Treatment
Common Antibiotics for treatment are:
- Sulfa/ Bactrim/ Sulfamethoxazole and Trimethoprim
- Ampicillin or Amoxicillin
- Cipro or Levaquin
- Doxycycline
- Trimethoprim
- Cephalosporins/ Keflex
- Nitrofurantoin/ Macrodantin/ Macrobid
Prevention of UTIs
The vast majority of young girls are taught to wipe urine and stool from front to back. This is to prevent the bacteria around the anus from being brought forward towards the vagina. The perineum is that area behind the vaginal opening and includes that area in front of the anus. The most common bacteria to cause a UTI are the enteric bacteria that grow on the perineum. Proper hygiene is the first line of defense against infections.
Anything that might irritate the vaginal area may lead to infections. Bubble baths in small children as well as perfumes, feminine hygiene sprays, and laundry detergents have been implicated. The irritated skin is more prone to bacterial colonization. The increased density of bacteria in that area leads to more opportunities for the bacteria to get into the bladder.
Since intercourse is a common time for bacteria to enter the urinary tract, it is advised that women wash before intercourse. Washing after intercourse may lower the infection rate by removing lubricant, bacteria, and semen. Urinating after intercourse should empty out any bacteria that entered the urethra. This helps to get rid of the bacteria before they have a chance to grow into an infection. In rare occasions, your doctor may give you an antibiotic to keep on hand to be taken immediately after intercourse. Usually a single dose of antibiotic will do in this situation. This single dose of antibiotic lowers the risk of yeast infection as well as any interference that antibiotics may cause with your birth control pills. Longer courses of antibiotics may lower the effectiveness of birth control pills.
Some studies show that there is an increase in bacterial adherence to the vaginal mucosa with changes in the hormones at different times in the menstrual cycle. Many women have told me that only at certain points in their cycle are they susceptible to UTIs with intercourse. Please tell your urologist if you have found a pattern to your UTIs.
Women also say that there is a difference in a UTI risk based on sexual position.
Some women relate the risk of a UTI to whether they use tampons versus pads. Usually, as long as they are changed regularly, it should not make a difference.
- Estrogen deficiency after menopause leads to vaginal dryness. This in turn leads to better adherence of bacteria to the skin and vaginal lining with increased risk of a UTI. The normal vaginal moisture contains factors that help prevent UTIs. Without this moisture and its antibodies, infections may increase in both number and severity. After stopping estrogen replacement therapy, there is an increase in UTIs.
- Incontinence leads to skin irritation and an increased risk of a UTI. This is likely due to the ammonia irritation of the skin with increased bacterial colonization.
- Cystoceles, also called prolapsed or dropped bladders, often occur after childbirth. The leftover urine increases in the bladder as the cystocele increases in size. This stagnant urine leads to an increased risk of a UTI.
- Diabetics have a decrease in their ability to fight infection and develop more frequent UTIs. Good control of your diabetes will reduce your UTI risk.
- Cotton panties absorb moisture better than nylon and may reduce your UTI risk.
- Water based lubricants work better than petroleum or silicone based lubricants for prevention of UTIs.
- Don’t douche. Douching washes away any protective factor that the normal vaginal secretions provide in preventing infection.
- Tight clothing such as tight jeans and pantyhose has been implicated.
- Do not continue to wear sweaty gym cloths any longer than necessary.
- Drink plenty of water.
- Spermicides alone or on condoms may cause UTIs.
- Diaphragm usage has been noted to increase the risk of UTIs more than other forms of birth control.
- Constipation may increase UTIs especially in children and the women of advanced age.
- An uncircumcised sex partner leads to an increased risk for getting UTIs. An unclean foreskin will harbor bacteria which can be transferred to the urethra.
Most Common Bacteria
These are the bacteria that normally live on the perineum. They are called enteric bacteria and are normal in the colon. E.coli is the most common of all bacteria to cause a UTI. E.coli accounts for 80 to 85% of uncomplicated UTIs. Other organisms include Klebsiella, Serratia, Providencia, Proteus, Enterococcus, Enterobacter, Pseudomonas, Staphylococcus, and Streptococcus.
Diagnosis
Urinalysis is the initial test for a UTI diagnosis. This begins with a chemical dipstick that changes color in the presence of blood, bacteria, and white blood cells (WBCs). These dipstick test results can be falsely positive if there is contamination from the urine flowing past the vagina. False positives also occur with yeast infections.
Microscopic urinalysis consists of placing 10-15cc of urine in a centrifuge for 10 minutes. The liquid is poured off, and the last drop is resuspended and placed on a microscope slide. Under 400-power magnification, the urine undergoes a white blood cell count (WBC), a red blood cell count (RBC), and an evaluation for crystals, bacteria, and epithelial cells. Epithelial cells are a sign of vaginal contamination and may invalidate a positive dipstick urinalysis.
Cultures are used to grow the bacteria in the laboratory under controlled conditions. If bacteria grow, then they are tested against antibiotics to determine the sensitivity of the bacteria. The bacteria are tested against multiple antibiotics. If serial cultures show the same bacteria over and over again, then it is thought that the original UTI has never cleared. If there are different bacteria on successive cultures, then it is felt that this is most likely a repeat infection. Multiple organisms indicate vaginal contamination. Lactobacillus is also felt to be due to vaginal contamination. Beta Strep is a normal perineal and vaginal bacterium and may be contamination, not a UTI. A positive culture from a voided specimen should contain 10 to the 5th power of colony forming units of a singe organism. Multiple organisms call into question that the specimen was contaminated and not a valid specimen. Catheterized specimens are positive at 10 to the 4th power CFU (colony-forming unit).
Specimen Collection
A voided urine specimen is obtained if possible. This is to try to avoid obtaining a catheterized specimen. Catheterization is the introduction of a small tube up the urethra into the bladder just far enough to get a urine specimen. Catheterization does avoid the risk of contamination.
A voided specimen may be obtained. While most women just urinate in a cup without proper cleaning, this is the worst possible specimen for accurate diagnosis. A proper specimen starts by cleaning with the antiseptic towelette. Cleaning should be all the way to the vaginal opening. With one hand, the vaginal lips or labia are held apart, and the cup is held in the other hand. A small spurt of urine will then wash away any lingering contamination. The midstream 2-3 ounces of urine are then caught in the specimen cup, with the remaining urine voided into the toilet.
UTI Treatment
The treatment of the UTI depends on whether it is classified as complicated or uncomplicated. An uncomplicated UTI is a simple bladder infection without fever or association with stones, catheters, or other complicating illnesses.
A complicated UTI is associated with fever >101°F, infection behind an obstructing kidney stone, or an infected catheter.
An uncomplicated UTI is treated with oral antibiotics. In young, healthy, college coed’s, studies have shown that 50% will clear with one dose of antibiotics. The problem is that 100% burned on urination or had other symptoms for 3 days. So therapy in healthy individuals should be limited to 3 days. If the woman has incomplete emptying, a history of failing to clear in 3 days, is diabetic or estrogen deficient, or is on immunosuppressant drugs, the treatment may be 5-7-10 or even 14 days.
A complicated UTI usually requires hospital admission with IV antibiotics. If associated with a kidney stone, the kidney will need to be unblocked before antibiotics can be effective.
Other Medications
- Pyridium or Phenazopyridine is an AZO dye, that when excreted in the urine, acts as a topical anesthetic.
- Methylene blue is a similar dye for topical anesthesia.
- Antispasmodics or anticholinergic medications used for overactive bladder are also effective in treating the bladder spasms so often associated with a UTI. These help with the frequency and urgency of urination until the antibiotic can kill the bacteria. Brand names are VESIcare, Enablex, Toviaz, Ditropan, Levbid, and Detrol.
Home Remedy
Drinking plenty of fluids will increase urine production and may flush out the bacteria, but rarely will your body be able to clear the infection.
Cranberry juice and tablets are reported to help treat and prevent a UTI. One study reported that if one drank 32 ounces of cranberry juice per day, there was a 20% reduction in the number of UTIs. That means if a woman has 5 UTIs per year the cranberry juice lowered that number from 5 to 4. Most people do not drink 32 oz of fluids per day in the first place. High intake of cranberry juice may cause kidney stones.
Taking a warm tub bath may relax the bladder spasms.
Ibuprofen and other NSAID medications are anti-inflammatory medications and may help relieve the pain of urination.
AZO over the counter is the same medication that is in prescription strength Pyridium. The dose has been reduced only from prescription strength 100mg to 95mg in the AZO over the counter.
Reports that pineapple juice relieves UTI symptoms are based on its purported anti-inflammatory effects on the bladder.